In emergency scenarios involving cardiac arrest or respiratory failure, knowing When should you start CPR (Cardiopulmonary Resuscitation) is crucial. The first line of defense is CPR, which is essential for maintaining blood flow and oxygenation. This essay thoroughly explores the complex situations that call for the use of CPR, emphasizing the value of quick response. As the main trigger for starting CPR, it is crucial to be skilled in identifying the absence of vital signs, especially the ceasing of breathing and pulse.
In general, some common scenarios are Unconsciousness, sudden cardiac arrest, choking, electrical injuries, drowning, drug overdose, and suffocation. When should you start CPR? By exploring these scenarios, we equip readers with knowledge based on evidence, allowing them to react to life-threatening events in an efficient manner. With this knowledge, people may considerably increase the chances of a successful outcome for persons in distress, emphasizing the crucial role that prompt CPR plays in saving lives. Moreover, we will have a look at devices that can help you perform CPR like automated external defibrillator (AED) and CPRmeter represented by Beatlife company.

Contents
How do I know if a person requires CPR?
A quick and thorough evaluation of a person’s responsiveness, breathing, and pulse is essential to determining When should you start CPR. First, try tapping and shouting for a response when you encounter a person who isn’t responding. If they do not respond, immediately dial emergency services or ask someone close by to do so to seek emergency medical help. Check for indications of typical breathing simultaneously by examining chest movement and listening for breath sounds. You should start CPR immediately if the person is not breathing or just breathing erratically.
Next, it’s critical to determine whether a pulse is present. Although difficult, especially in high-stress circumstances, pulse checks are crucial for determining whether CPR is necessary. Chest compressions should be started if you are skilled at pulse assessment and cannot discover a pulse in 10 seconds. Use the right method to locate and feel the carotid artery in the neck or the radial artery on the wrist to check someone’s pulse before starting Cardiopulmonary Resuscitation (CPR). Keep your touch mild to avoid vascular compression.
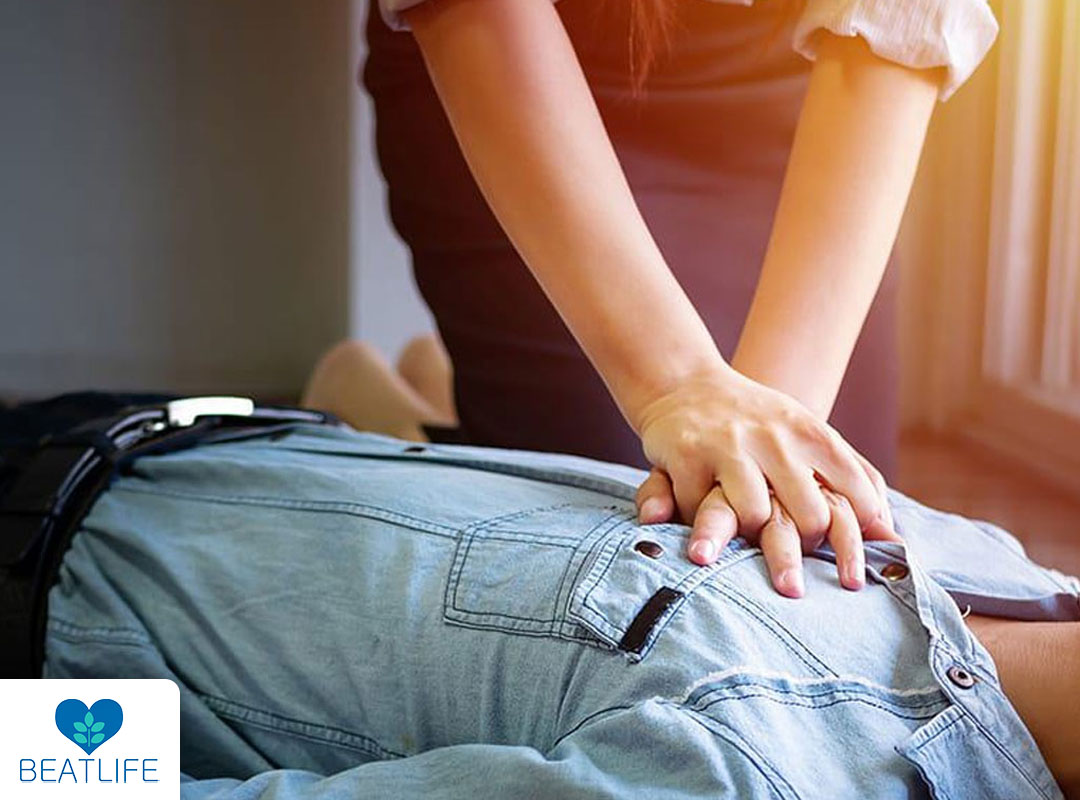
So when should you start CPR? Chest compressions should be started as soon as you realize no regular breathing is occurring and you either cannot feel a pulse or are doubtful. Place your hands correctly on the chest, apply compressions between 100 and 120 times per minute, and let the chest fully extend between compressions. If you are proficient in CPR and can provide rescue breaths, add them to the cycle by giving two breaths every 30 compressions. Until professional medical assistance arrives, the patient starts breathing independently, or you become too exhausted to continue, repeat this cycle of compressions and breaths. Throughout, keep your technique steady and rhythmic.
When should you start CPR?
let’s discuss different scenarios in the context of When should you start CPR:
- In a state of unconsciousness: The first thing to do if you encounter an unconscious person is to see if they are responding. To see if the person wakes up or reacts in any way, tap and shout at them. CPR should be started immediately if the person is still not breathing properly or has no pulse. Any number of factors, such as diseases, head injuries, or intoxication, can lead to unconsciousness, and CPR can be an essential intervention to maintain vital functions.
- Cardiac arrest: Cardiac arrest is when the heart stops functioning properly, stopping the flow of blood. In such circumstances, the person stops breathing and loses consciousness. Up until an AED is accessible or emergency medical assistance comes, CPR is crucial to keep the blood flowing. Early CPR can considerably increase the likelihood that you will successfully restore a normal cardiac rhythm.
- Choking: Due to oxygen depletion, someone choking and unable to breathe or cough properly risks losing consciousness. If the person becomes unconscious in these circumstances, CPR may be required. However, the Heimlich maneuver or abdominal thrusts to remove the obstruction are the first line of treatment for choking. CPR with chest compressions should be started once the person loses consciousness.
- Electrocution: Electrical damage can alter the heart’s rhythm and cause cardiac arrest. It’s When should you start CPR if you come across someone who has been electrocuted and is unresponsive with no pulse. Ensure the power source is safely disconnected to avoid further damage.
- Drowning: Due to water getting in the airways, drowning can cause someone to cease breathing and lose consciousness. If you encounter a drowning victim who is not breathing, start CPR immediately. While water is being evacuated from the airway, effective chest compressions can assist in circulating oxygenated blood to essential organs.
- Drug Overdose: Some drug overdoses, particularly opioid overdoses, can result in respiratory failure, which makes a person unresponsive and stop breathing. In these circumstances, CPR may be required to sustain oxygenation until the medications’ effects wear off or emergency medical help comes.
The main factor that ties these situations together is the possibility of reduced oxygenation and circulation, which calls for the quick start of CPR when the victim is unconscious, not breathing properly, or has no pulse. In these life-threatening situations, immediate CPR can dramatically increase the probability of survival and be a vital link to more sophisticated medical interventions.

When should you not perform CPR?
Equally important to knowing when to start CPR is knowing when not to. There are certain circumstances in which performing CPR would be ineffective or inappropriate. First and foremost, medical professionals should respect the requests of patients who have a legal Do Not Resuscitate (DNR) order and cease CPR attempts. DNR orders are created when someone consciously chooses not to receive aggressive life-saving interventions, frequently due to terminal illnesses or bleak prognoses. Furthermore, CPR should not be performed if a person exhibits clear indications of demise, such as rigor mortis, decomposition, or severe injuries incompatible with life. Further attempts at resuscitation in this situation are not only unsuccessful but also possibly unethical and harmful from a medical standpoint.
Additionally, prolonged arrests that go unnoticed or situations in which a long period has gone after the cardiac or respiratory event may make CPR less effective, resulting in discontinuance. Finally, judgments on CPR are influenced by the futility principle and respect for the patient’s wishes regarding their end-of-life. In the end, the choice to stop CPR should be decided in conjunction with medical specialists, while also honoring the patient’s advanced wishes and the particulars of the incident. It emphasizes how crucial effective communication, advanced care planning, and medical ethics are when making decisions about end-of-life care.
What equipment can be used in CPR?
Cardiopulmonary Resuscitation (CPR) normally does not require specific equipment and is essentially manual. However, there are a few instruments and gadgets that can help with CPR administration:
- CPR Mask or Face Shield: During rescue breaths, these tools build a barrier between the rescuer’s mouth and the victim’s mouth, lowering the risk of disease transmission and enabling a stronger seal.
- Automated External Defibrillator (AED): AEDs, which are frequently found in public settings but are not directly associated with CPR, can be used to evaluate the heart’s rhythm and, if necessary, administer an electric shock to return the heartbeat to normal.
- CPR Feedback Devices: These instruments, like the CPRmeter, offer instant feedback regarding the depth and frequency of chest compressions. For instance, the CPRmeter provided by the BEATLIFE company is a tool that ensures the proper depth and pace of chest compressions during CPR, improving their efficacy.
- Bag-Valve-Mask (BVM) Resuscitator: When performing CPR with rescue breaths, healthcare personnel can use this gadget with a bag and a mask to help ventilate.
- Chest Compression Devices: Automated chest compression systems, which can administer constant chest compressions, may be employed in some high-tech medical settings, although they are not frequently used outside hospitals.
It’s crucial to remember that while these instruments may aid medical professionals or improve CPR quality, effective CPR fundamentally relies on strong chest compressions and, when necessary, adequate rescue breaths. During CPR, prompt action, appropriate technique, and quick availability of qualified medical assistance are crucial.
What are the Post-CPR Supports?
An essential part of the whole care given to patients who have experienced cardiac arrest and received CPR is post-CPR support. Even though performing CPR successfully can greatly boost a victim’s chances of survival, survivors frequently need urgent medical attention as well as continuous support. It is crucial that people have a professional medical examination following the intervention in order to determine any underlying causes of the cardiac arrest and to handle any potential sequelae. In order to protect the patient’s wellbeing and prevent more cardiac episodes, post-CPR care includes diagnostic testing, monitoring, and interventions by medical personnel.
The emotional and psychological health of the survivor and their loved ones is just as important as the physical health. Being in cardiac arrest can be a frightening experience, and people may suffer from PTSD, depression, anxiety, or a dread of it happening again. Post-CPR assistance should include information, support groups, and psychological counseling to assist survivors and their families in coping with the emotional consequences. Creating a strong support system with medical professionals, mental health specialists, and community resources is essential to promoting the full recovery of those who have received CPR.
Reviewed by Dr Jamshidi Mohammad Reza

